The MIGHT study at Michigan Medicine is a groundbreaking project that aims to address the pressing need for increased rates of genetic testing for identifying hereditary cancer. With the prevalence of cancer on the rise and the growing recognition of the role that genetics play in its development, this study comes at a crucial time. By actively seeking participants who have been diagnosed with cancer or have a family history of cancer, the researchers are able to gather valuable data that can potentially revolutionize cancer care.
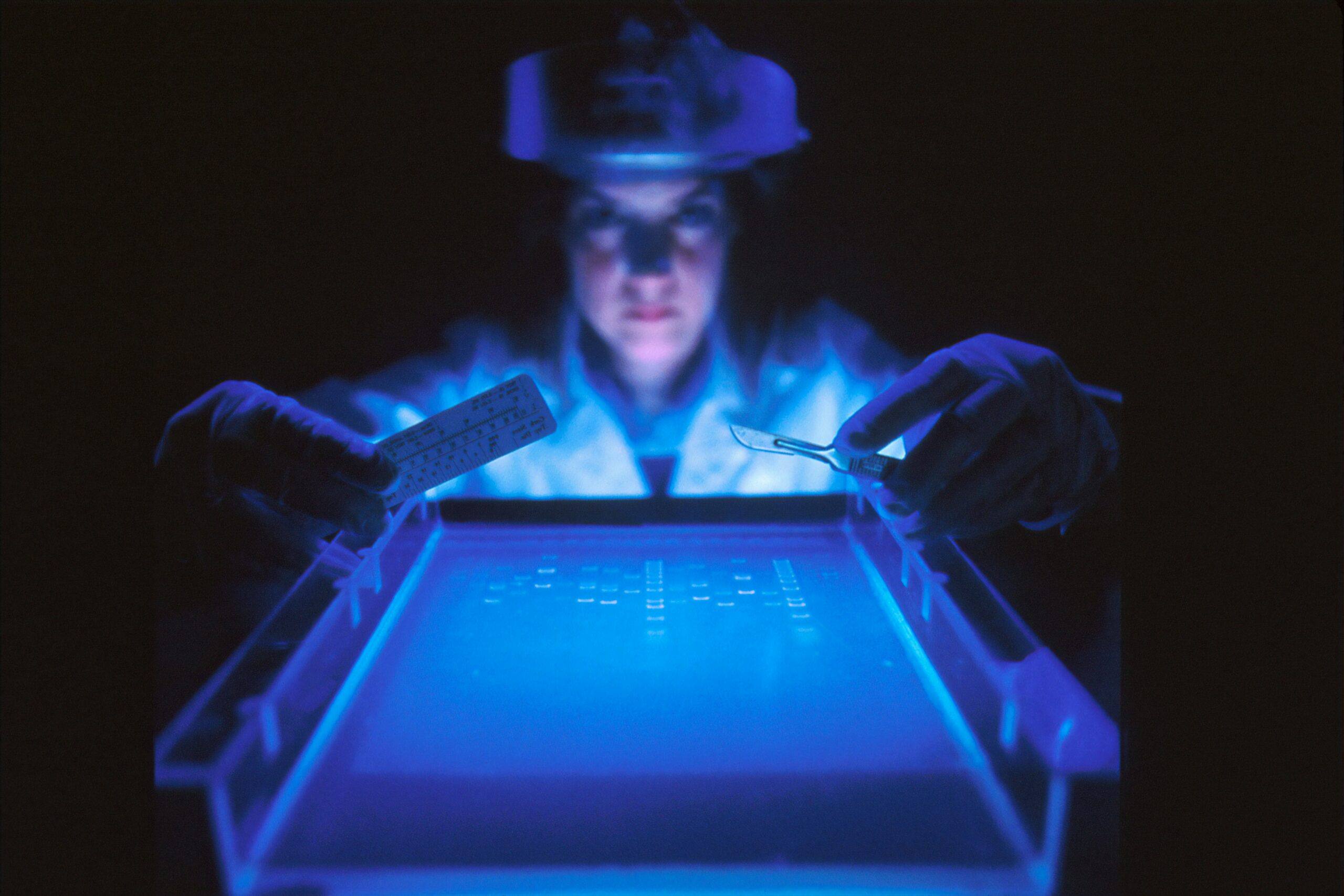
Genetic testing has emerged as a powerful tool in the fight against cancer. By analyzing an individual’s DNA, it is possible to identify specific genetic mutations that may increase the risk of developing certain types of cancer. This information can then be used to guide personalized treatment plans and preventive measures, such as earlier and more frequent cancer screenings.
The MIGHT study is particularly significant because it focuses on increasing rates of genetic testing specifically for hereditary cancers. These are types of cancer that have a strong familial component, meaning they tend to run in families due to inherited genetic mutations. By identifying individuals who are at a higher risk of developing hereditary cancers, healthcare providers can implement targeted screening strategies and interventions to detect and treat these cancers at earlier stages.
The $4 million grant from the National Institutes of Health’s Cancer Moonshot program has provided the necessary funding for the MIGHT study to make significant strides in the field of genetic testing for cancer. This generous funding has allowed researchers to recruit a large and diverse group of participants, ensuring that the study’s findings are applicable to a wide range of populations.
Since its inception in 2020, the MIGHT study has made substantial progress in its mission to increase rates of genetic testing for cancer. The researchers have developed innovative strategies to overcome barriers to testing, such as cost, accessibility, and awareness. They have partnered with various healthcare providers, genetic counselors, and community organizations to raise awareness about the importance of genetic testing and to provide resources and support for individuals considering testing.
Furthermore, the MIGHT study has implemented educational initiatives to enhance genetic literacy among both healthcare professionals and the general public. By increasing understanding and awareness of the benefits and implications of genetic testing, the study aims to empower individuals to make informed decisions about their own health and the health of their families.
The impact of the MIGHT study is far-reaching. Not only does it have the potential to improve outcomes for individuals and families affected by hereditary cancers, but it also contributes to the broader field of cancer research. By gathering data on genetic mutations and their associations with specific types of cancer, the study can contribute to the development of targeted therapies and interventions that may ultimately lead to more effective treatments and improved survival rates.
In conclusion, the Michigan Genetic Hereditary Testing (MIGHT) study at Michigan Medicine is a groundbreaking project that aims to increase rates of genetic testing for hereditary cancers. With its focus on identifying individuals at a higher risk of developing these cancers, the study has the potential to revolutionize cancer care and improve outcomes for countless individuals and families. Through its innovative strategies, educational initiatives, and collaboration with various stakeholders, the MIGHT study is paving the way for a future where genetic testing becomes a routine part of cancer prevention and treatment.
Understanding the Role of Genetic Factors in Cancer
While most cancer cases occur by chance, approximately 1 in every 10 cancer diagnoses can be attributed to an underlying genetic factor. Dr. Elena Stoffel, Associate Professor of Internal Medicine at the University of Michigan and Director of the Rogel Cancer Center’s Genetics Clinic, explains the significance of identifying individuals with a predisposition to developing cancer. Early intervention can lead to earlier detection or even prevention through screenings and behavioral interventions.
Genetic factors play a crucial role in the development of cancer. These factors can be inherited from one or both parents and can increase the risk of certain types of cancer. For example, mutations in the BRCA1 and BRCA2 genes are known to increase the risk of breast and ovarian cancer. Identifying individuals with these mutations can help healthcare professionals develop personalized screening and prevention strategies.
Genetic testing has become an essential tool in identifying individuals at risk of developing cancer. This type of testing involves analyzing a person’s DNA to look for specific genetic alterations or mutations that are associated with an increased risk of cancer. By identifying these genetic factors, healthcare professionals can provide individuals with personalized recommendations for screenings and interventions.
Early intervention is crucial when it comes to cancer. By identifying individuals with a genetic predisposition to cancer, healthcare professionals can implement regular screenings at an earlier age or more frequently. This allows for the detection of cancer at its earliest stages when treatment options are often more effective. Additionally, individuals with a higher risk of developing cancer can be educated about lifestyle changes that can reduce their risk, such as maintaining a healthy weight, exercising regularly, and avoiding tobacco and excessive alcohol consumption.
Furthermore, genetic factors can also influence treatment decisions. Certain genetic mutations can affect how a person’s body metabolizes certain medications, making them more or less effective. By understanding a person’s genetic makeup, healthcare professionals can tailor treatment plans to maximize their effectiveness and minimize potential side effects.
In conclusion, genetic factors play a significant role in the development of cancer. Identifying individuals with a genetic predisposition to cancer allows for early intervention, which can lead to earlier detection or even prevention. Genetic testing has become an essential tool in personalized medicine, enabling healthcare professionals to develop tailored screening and treatment plans. By understanding the role of genetic factors in cancer, we can continue to make strides in cancer prevention and treatment.
The MIGHT Study and its Interventions
The MIGHT study invites anyone interested to complete a family cancer history form. Based on their family history, participants who meet the criteria for genetic testing may be eligible to join a randomized trial. These participants will be assigned to one of two intervention arms:
- Contacted in-person or over the telephone by a genetics health coach
- Given a link to a virtual genetics navigator
In both intervention arms, participants will receive information about the importance of genetic testing, its impact on health, and answers to commonly asked questions. Genetic testing can be conducted using cheek swabs or blood testing. Clinical genetic testing for cancer susceptibility is performed by specialized clinical genetics laboratories, which provide results regarding alterations in specific cancer susceptibility genes that may require specialized management.
The in-person or telephone intervention arm involves participants being contacted by a genetics health coach. These coaches are trained professionals who specialize in genetics and provide personalized guidance and support to individuals undergoing genetic testing. They offer a comprehensive assessment of the participant’s family cancer history and explain the potential implications of genetic testing based on the identified risk factors. The genetics health coach also addresses any concerns or fears the participant may have and helps them make informed decisions regarding their participation in the study.
On the other hand, the virtual genetics navigator intervention arm offers participants a link to an online platform that provides guidance and information on genetic testing. This virtual genetics navigator serves as a digital resource that participants can access at their convenience. It offers interactive modules and educational materials that cover various aspects of genetic testing, including the science behind it, the different types of tests available, and the potential benefits and limitations. Participants can navigate through the platform at their own pace, gaining a comprehensive understanding of genetic testing and its implications for their health.
Regardless of the intervention arm, all participants will receive detailed information about the genetic testing process. They will learn about the different methods of sample collection, such as cheek swabs or blood testing, and the subsequent analysis performed by specialized clinical genetics laboratories. These laboratories have the expertise to identify alterations in specific cancer susceptibility genes that may require specialized management. The results of the genetic testing will be communicated to the participants, along with appropriate recommendations for further medical follow-up based on the identified genetic alterations.
The MIGHT study aims to empower individuals by providing them with the necessary knowledge and support to make informed decisions about genetic testing. By offering both in-person and virtual interventions, the study caters to the diverse needs and preferences of participants. Ultimately, the goal is to enhance the understanding of genetic testing for cancer susceptibility and its potential impact on health, leading to improved prevention, early detection, and management strategies for individuals and their families.
Benefits of Genetic Testing and Specialized Management
Individuals identified through genetic testing as having alterations in cancer susceptibility genes may benefit from extra preventative measures. These measures can help doctors detect cancer earlier and potentially intervene at an earlier stage. Examples of specialized management include more frequent breast cancer screenings, earlier colon cancer screenings, or other interventions aimed at detecting cancers early or preventing their development in individuals at high risk.
Even those who do not meet the criteria for genetic testing in the MIGHT study are encouraged to discuss the possibility of genetic testing with their healthcare provider. The potential benefits of genetic testing, including early detection and prevention, make it an important consideration for individuals with a family history of cancer.
Genetic testing has revolutionized the field of medicine by providing valuable insights into a person’s risk of developing certain diseases, including cancer. By analyzing an individual’s DNA, genetic testing can identify specific alterations or mutations in genes that are associated with an increased susceptibility to cancer. This information is crucial in determining appropriate management strategies for individuals at high risk.
One of the major benefits of genetic testing is the ability to detect cancer at an early stage. For individuals identified as having alterations in cancer susceptibility genes, specialized management can be implemented to ensure regular and more frequent screenings. For example, women with a BRCA1 or BRCA2 mutation, which are genes associated with an increased risk of breast and ovarian cancer, may undergo more frequent mammograms and breast MRIs to detect any abnormalities at an early stage. Similarly, individuals with alterations in genes associated with colon cancer may undergo earlier and more frequent colonoscopies to detect any precancerous polyps or tumors.
In addition to early detection, genetic testing also allows for targeted interventions aimed at preventing the development of cancer. For individuals at high risk, preventive measures such as prophylactic surgery or chemoprevention drugs may be recommended. Prophylactic surgery involves the removal of organs or tissues that are at a high risk of developing cancer. For example, women with a BRCA1 or BRCA2 mutation may choose to undergo a prophylactic mastectomy to reduce their risk of developing breast cancer. Chemoprevention drugs, on the other hand, are medications that can reduce the risk of developing certain types of cancer. These interventions can significantly reduce the likelihood of cancer development and improve overall outcomes for individuals at high risk.
It is important to note that genetic testing is not only beneficial for those who meet the criteria for testing in specific studies or research projects. Even individuals who do not meet these criteria but have a family history of cancer should consider discussing the possibility of genetic testing with their healthcare provider. Genetic testing can provide valuable information about an individual’s risk of developing cancer, allowing for appropriate management and preventive strategies to be implemented. Early detection and prevention are key in the fight against cancer, and genetic testing plays a crucial role in achieving these goals.